Reherniated Disc Specialist
If you are struggling with symptoms of lumbar disc reherniation, such as recurrent back pain or sciatica, or if you are experiencing new symptoms following spinal surgery, it’s crucial to seek expert care promptly. Dr. Andre M. Samuel, orthopedic spine specialist, provides comprehensive evaluations and tailored treatment plans for patients in the Clear Lake, Houston, Sugar Land, TX area who have been diagnosed with lumbar disc reherniation or a failed discectomy. Contact Dr. Samuel’s team today to schedule a consultation and explore both non-surgical and surgical options.

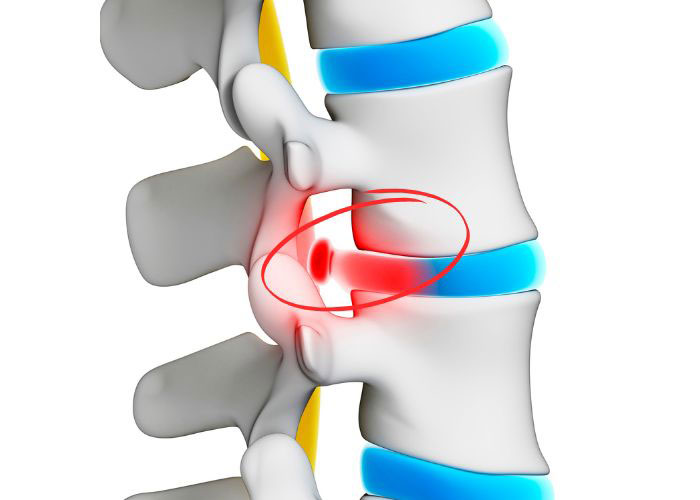
What is lumbar disc re-herniation?
When a disc in the lower back herniates again after surgery it’s referred to as a lumbar disc reherniation. Up to 15% of patients who undergo a discectomy to remove part of a herniated disc experience this issue, resulting in the return of persistent back and leg pain. A reherniation is part of a broader condition known as failed back surgery syndrome (FBSS). Identifying the precise cause of the pain—re-herniation, scar tissue, or a new herniation—is crucial for proper treatment. Doctor Andre M. Samuel, orthopedic spine specialist, treats patients in the Clear Lake, Houston, Sugar Land, TX area suffering from lumbar disc re-herniation or a failed discectomy.
What are the common causes of lumbar disc re-herniation?
Various factors can lead to a lumbar disc reherniation or a failed discectomy. Primary causes include:
- Incomplete removal of all the herniated or damaged disc material.
- Ongoing degeneration of the disc and adjacent discs.
- Physical activity performed too early after surgery.
Scar tissue formation can occur after surgery, compressing nerve roots and causing symptoms similar to those of a herniated disc. That’s why it’s crucial to consult with an expert like Dr. Samuel, who can evaluate your condition and accurately determine the cause of any re-herniation.
Who is more susceptible to lumbar disc re-herniation?
Some patients are more susceptible to lumbar disc reherniation following surgery than others. Younger patients tend to recover better from surgery than older adults who are more prone to degenerative disc changes, causing more complications. Factors leading to more complications include:
- Individuals with weak core muscles and low overall fitness levels may face greater challenges in recovery.
- Jobs that require heavy lifting, bending, or twisting can increase the risk of reherniation and other complications.
- Smoking and obesity negatively impact tissue healing and overall spinal health, exacerbating recovery issues.
- Variations in genes related to collagen and other structural components of the spine can also influence susceptibility to complications.
What are the first signs or symptoms of lumbar disc degeneration?
Signs of lumbar disc reherniation can be similar to the symptoms a patient experienced before surgery. They include:
- A resurgence of back pain that subsided after surgery.
- Sciatica pain that radiates from the lower back down to the buttocks and legs.
- Numbness or tingling in the legs or feet
- Muscle weakness in the lower extremities, making it hard to stand up from a seated position or walk.
- Decreased range of motion in the lower back, with difficulty bending or twisting.
A patient experiencing any of these systems after spinal surgery needs to be evaluated for possible treatment interventions. Any new symptoms such as changes in reflexes, bowel or bladder function, are considered emergencies and require immediate medical attention.
How is lumbar degenerative disc disease diagnosed?
Dr. Samuel will review your medical history and conduct a physical exam in the office to assess nerve function and pain. He will order imaging studies such as an MRI to visualize the spine, discs, and soft tissues to determine if any post-surgical changes have occurred. Sometimes more specific diagnostic testing may be ordered including nerve conduction studies which help confirm the source of symptoms and help Dr. Samuel and his team develop a treatment plan.
What is the treatment for lumbar disc reherniation?
Treatment for lumbar disc reherniation or a failed discectomy often starts with conservative or non-surgical options, especially if the symptoms are manageable. Dr. Samuel may recommend one or more of the following options, before another surgery.
Non-surgical options:
- Physical therapy to strengthen the back, improve flexibility, and reduce pressure on the nerves.
- Pain relievers, anti-inflammatories, and muscle relaxants to manage pain and inflammation.
- Corticosteroid injections around the affected nerve root to reduce inflammation and pain.
If a conservative approach does not provide a patient with pain relief, surgery may be the only way to help relieve the discomfort and restore function. There are several different surgical options including:
Surgical Options:
- Revision discectomy – Removes the reherniated disc material.
- Spinal Fusion – Joins two vertebrae to eliminate motion and reduce pain.
- Laminectomy – Removes part of the vertebra to relieve pressure on the spinal nerves.
A less common procedure replaces the damaged disc with an artificial one. The choice of treatment depends on the patient’s overall health, how severe the disc damage is, and the response to previous treatments. Dr. Samuel discusses all viable options for each patient, explaining the pros, cons, and risks.



